1. Introduction: Timing Is Everything in Skin Treatments
Laser technology continues to evolve in dermatology, driven by the need for greater precision, safety, and efficacy. One key factor shaping outcomes is pulse duration—the length of time a laser emits energy. This small detail has a major impact on how the skin responds. The shift from nanosecond to picosecond laser technology marks a major advancement in aesthetic and medical dermatology. Picosecond lasers deliver ultra-short pulses—up to ten times faster than nanosecond lasers—producing more targeted results with less heat and downtime. This speed has revolutionized treatments for tattoos, pigmentation, acne scars, and signs of aging, offering faster healing and improved comfort. For both dermatologists and patients, understanding how laser speed affects results is essential. In this blog, we’ll explore how the difference between nanosecond and picosecond lasers goes far beyond timing—it influences everything from treatment depth to skin safety.
2. Understanding the Basics: What Is Pulse Duration?
Before delving into the comparative advantages of different laser technologies, it’s essential to establish a foundational understanding of pulse duration and its clinical implications. Pulse duration represents the temporal window during which laser energy is delivered to target tissues, fundamentally influencing how that energy interacts with chromophores and surrounding structures.
2.1 The Science of Laser Pulse Duration
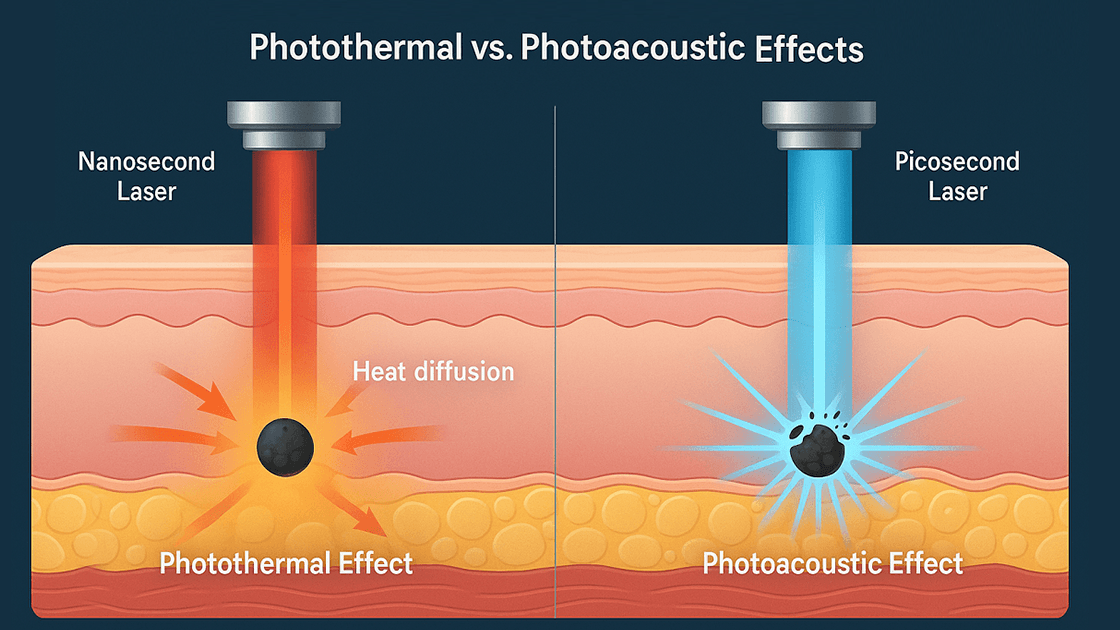
Pulse duration, measured in units of time ranging from continuous wave to femtoseconds, defines the temporal characteristics of laser energy delivery. In dermatological applications, the most relevant timeframes span from milliseconds (10⁻³ seconds) to picoseconds (10⁻¹² seconds). The selection of appropriate pulse duration directly influences the balance between photomechanical and photothermal effects within target tissues. Picosecond lasers operate within the subnanosecond range, providing greater photomechanical effects and less heat diffusion into neighboring structures.
2.2 How Pulse Duration Impacts Tissue Interaction
The interaction between laser energy and biological tissues follows complex biophysical principles governed by chromophore absorption, heat generation, and energy dissipation mechanisms. Shorter pulse durations favor photomechanical disruption over thermal coagulation, enabling more precise targeting of specific cellular components while minimizing collateral damage. This principle becomes particularly relevant when treating delicate facial structures or patients with darker skin phototypes where thermal injury risk is elevated.
2.3 Why Thermal Relaxation Time (TRT) Matters
Thermal relaxation time represents the time required for a heated structure to cool to half its peak temperature, with smaller objects cooling faster than larger ones. Understanding TRT is fundamental to laser safety and efficacy, as it determines the optimal pulse duration for selective photothermolysis. When laser pulses are delivered within or shorter than the target’s TRT, heat remains confined to the intended chromophore, minimizing damage to surrounding tissues and reducing adverse effects.
3. Picosecond Lasers: A Leap Forward in Dermatology
The introduction of picosecond laser technology has revolutionized dermatological treatments by harnessing ultrashort pulse durations to achieve unprecedented precision and efficacy. These advanced systems operate on fundamentally different principles compared to their nanosecond counterparts, offering unique advantages across multiple clinical applications.
3.1 How Picosecond Lasers Work
Picosecond lasers generate extremely brief pulses of intense light energy, typically lasting between 450 to 750 picoseconds depending on the specific wavelength and system design. This ultrashort duration creates primarily photomechanical effects rather than thermal damage, resulting in the fragmentation of target chromophores through acoustic shockwaves and cavitation effects. The mechanism involves rapid heating and expansion of pigment particles, creating pressure waves that mechanically disrupt the target while preserving surrounding tissue integrity through minimal heat diffusion.
3.2 Clinical Applications of Picosecond Lasers
Picosecond laser technology has broadened clinical indications to include treatment of benign pigmented lesions, photodamage, melasma, acne scarring, and tattoo removal. The versatility of these systems stems from their ability to target multiple chromophores across different wavelengths, including melanin, hemoglobin, and exogenous tattoo pigments. Advanced picosecond platforms often incorporate diffractive lens arrays or fractional handpieces to create controlled micro-injuries that stimulate collagen remodeling for skin rejuvenation applications.
3.3 Key Advantages Over Nanosecond Lasers
The superiority of picosecond technology manifests in several critical areas: enhanced pigment clearance efficiency, reduced treatment sessions, improved safety profiles in darker skin types, and expanded treatment capabilities. The photomechanical mechanism of action allows for more effective fragmentation of resistant pigments, particularly beneficial for multicolored tattoos and recalcitrant melasma cases. Additionally, the minimal thermal component reduces post-inflammatory hyperpigmentation risk, making these systems safer for Fitzpatrick skin types IV-VI where thermal injury could exacerbate pigmentary concerns.

4. Nanosecond Lasers: The Reliable Classic
Despite the advancement of picosecond technology, nanosecond Q-switched lasers continue to play a vital role in dermatological practice. These established systems have decades of clinical evidence supporting their efficacy and safety across numerous indications, making them indispensable tools in the dermatologist’s armamentarium.
4.1 How Nanosecond Lasers Operate
Nanosecond lasers deliver energy pulses lasting between 5 to 20 nanoseconds, generating predominantly photothermal effects through rapid chromophore heating and subsequent thermal expansion. The mechanism relies on selective photothermolysis principles, where specific wavelengths target melanin, hemoglobin, or tattoo pigments while maintaining pulse durations within the thermal relaxation time of target structures. This approach has proven highly effective for various pigmentary and vascular lesions, establishing the foundation for modern laser dermatology.
4.2 When Nanosecond Lasers Still Shine
Nanosecond Q-switched lasers remain the gold standard for certain clinical applications, particularly in treating superficial pigmented lesions, solar lentigines, and café-au-lait macules. Their established efficacy, predictable outcomes, and extensive safety data make them excellent choices for straightforward cases where the additional benefits of picosecond technology may not justify the increased cost. Many practitioners continue to rely on nanosecond systems for routine pigmentation treatments, especially in clinical settings where cost-effectiveness is prioritized over cutting-edge technology.
4.3 Drawbacks Compared to Picosecond Technology
The limitations of nanosecond lasers become apparent when treating complex pigmentary disorders, resistant tattoo pigments, or patients requiring multiple wavelengths for comprehensive treatment. The predominantly thermal mechanism can increase the risk of post-inflammatory hyperpigmentation, particularly in darker skin types, and may require more treatment sessions to achieve optimal clearance. Additionally, the thermal component limits treatment density and may necessitate longer healing periods between sessions, potentially extending overall treatment timelines.
5. Comparing Side-by-Side: Which Laser Wins Where?
| Feature | Picosecond Laser | Nanosecond Laser |
| Pulse Duration | ~10⁻¹² seconds (trillionths of a second) | ~10⁻⁹ seconds (billionths of a second) |
| Primary Mechanism | Photoacoustic effect (mechanical shock) | Photothermal effect (heat-based) |
| Tissue Impact | Minimal heat, less damage to surrounding tissue | More heat, higher risk of collateral tissue damage |
| Efficacy in Tattoo Removal | Highly effective for multicolored, stubborn, and previously treated tattoos | Effective for black and dark blue ink; less effective for multicolored tattoos |
| Pigment Treatment | Effective on dermal and mixed-type pigment (e.g., melasma, PIH) | Better for superficial pigment (e.g., freckles, age spots) |
| Skin Rejuvenation | Stimulates collagen; improves texture, tone, and acne scars | Limited collagen stimulation; rarely used for skin rejuvenation |
| Sessions Required | Fewer sessions needed due to higher efficacy per treatment | More sessions typically required for similar results |
| Downtime | Minimal; most patients return to routine quickly | Moderate; more redness and risk of swelling or PIH |
| Risk for Darker Skin Types | Lower risk of post-inflammatory hyperpigmentation; safer for Fitzpatrick IV–VI | Higher risk of PIH; caution advised for darker skin tones |
| Comfort Level | Generally well-tolerated; may cause brief snapping sensation | Can feel more intense due to thermal effects |
| Device Cost (for clinics) | Higher initial investment | Lower cost; more widely available |
| Best For | Acne scars, melasma, multicolored tattoos, skin rejuvenation | Black tattoos, freckles, lentigines, superficial pigment |
6. Clinical Considerations: Matching the Right Laser to the Right Patient
Optimal laser selection requires comprehensive patient assessment, clear treatment objectives, and thorough understanding of each technology’s capabilities and limitations. The decision-making process must incorporate multiple variables to ensure safe, effective, and cost-appropriate treatment plans.
6.1 Who Benefits More from Picosecond Laser Treatments?
Mixed or Colored Tattoos
Patients presenting with professional tattoos containing multiple colors, particularly blues, greens, purples, and yellows, benefit significantly from picosecond technology. The enhanced photomechanical disruption mechanism effectively fragments resistant pigments that absorb poorly at traditional Q-switched wavelengths. Additionally, layered or coverup tattoos with complex pigment mixtures respond more favorably to the superior penetration and fragmentation capabilities of picosecond systems.
Fitzpatrick IV–VI Skin Types
Individuals with darker skin phototypes face increased risks of post-inflammatory hyperpigmentation and thermal injury with traditional laser treatments. Picosecond lasers offer enhanced safety profiles through reduced thermal diffusion and more precise energy delivery, making them ideal for treating pigmentary disorders in ethnic populations. The photomechanical mechanism minimizes heat generation while maintaining therapeutic efficacy for melasma, post-inflammatory hyperpigmentation, and benign pigmented lesions.
Acne Scars, Age Spots, or Melasma
Patients seeking comprehensive skin rejuvenation benefit from picosecond technology’s ability to simultaneously address multiple concerns through various treatment modalities. The versatility of modern picosecond platforms enables practitioners to customize treatments for specific indications, whether targeting discrete pigmented lesions, stimulating collagen remodeling for scar revision, or providing overall skin texture improvement through controlled micro-injury patterns.
6.2 Cost, Comfort, and Accessibility
The economic considerations surrounding laser technology adoption significantly impact treatment accessibility and clinical decision-making. Picosecond laser systems typically require higher initial capital investments and may have increased per-treatment costs compared to established nanosecond platforms. However, the potential for reduced treatment sessions and enhanced outcomes may offset higher upfront costs through improved patient satisfaction and practice efficiency. Patient comfort during and after treatment represents another crucial consideration, with picosecond lasers generally offering reduced discomfort due to minimal thermal effects and shorter treatment times. The decreased risk of adverse effects and faster healing may also improve patient compliance and treatment completion rates.
6.3 What Experts Say: It’s Not One-Size-Fits-All
Leading dermatologists and laser specialists emphasize that optimal treatment outcomes depend on matching appropriate technology to specific clinical scenarios rather than universally adopting newer systems. Systematic reviews have established picosecond lasers as safe and effective treatment modalities for an increasing range of dermatologic indications, while acknowledging that nanosecond systems continue to provide excellent results for many traditional applications. Expert consensus suggests that successful laser practices often incorporate both technologies to maximize treatment options and optimize outcomes across diverse patient populations. The decision between picosecond and nanosecond systems should be based on evidence-based medicine principles, considering individual patient factors, treatment objectives, and available resources rather than technology trends alone.
7. Patient Safety: Minimizing Risks and Maximizing Results
7.1 Pre-Treatment Evaluation: The Foundation of Safe Laser Use
A comprehensive assessment is essential before initiating any laser treatment. This includes reviewing medical history, current medications, sun exposure habits, and establishing realistic expectations. Special attention should be given to contraindications such as photosensitizing drugs, recent isotretinoin use, active infections, and pregnancy. Additionally, skin phototyping using the Fitzpatrick scale helps guide laser wavelength selection, fluence settings, and aftercare planning.
7.2 In-Treatment Protocols: Precision Prevents Complications
During the procedure, safety begins with proper eye protection for both the patient and clinician. Performing a test spot, using conservative energy levels, and gradually adjusting parameters are crucial in minimizing risks. These protocols help reduce thermal damage and increase patient comfort, especially in sensitive or darker skin types.
7.3 Post-Treatment Care: Healing with Caution and Clarity
Aftercare instructions play a pivotal role in outcome quality. Patients should be advised to avoid sun exposure, use gentle skincare products, and monitor their skin for any unusual reactions. Emphasizing sun protection and soothing topical care helps accelerate recovery and minimize adverse effects such as erythema or post-inflammatory hyperpigmentation.
7.4 Follow-Up Matters: Monitoring Enhances Results
Ongoing follow-up appointments enable practitioners to assess treatment efficacy, track healing progress, and identify any delayed side effects. These visits also help refine future treatment plans and ensure long-term patient satisfaction.
8. Conclusion: Faster Pulses, Better Outcomes
The shift from nanosecond to picosecond laser technology marks a major advancement in dermatology—delivering enhanced precision, safety, and broader clinical utility. Picosecond lasers excel in treating complex pigmentary conditions, multicolored tattoos, and darker skin tones thanks to their photomechanical action, which minimizes heat damage and improves pigment clearance. These benefits lead to fewer sessions, reduced side effects, and higher patient satisfaction. Yet, nanosecond lasers still offer reliable, cost-effective results for many standard applications. Ultimately, the best choice depends on individual patient needs, treatment goals, and clinical context. Successful outcomes rely not just on having advanced technology, but on using it wisely. In laser dermatology, pulse speed isn’t just a technical spec—it defines safety, results, and patient experience. Picosecond lasers open exciting new frontiers, but thoughtful integration of both technologies ensures the best care for every patient.
9. FAQs
Generally, picosecond laser treatments are less painful due to reduced thermal effects and shorter treatment times. The photomechanical mechanism creates less heat, resulting in decreased discomfort during and after treatment.
For tattoo removal, picosecond lasers typically require 20-40% fewer sessions depending on tattoo characteristics. For pigmented lesions, the reduction may be less dramatic but still clinically significant.
Picosecond lasers have improved safety profiles for darker skin types (Fitzpatrick IV-VI) due to reduced thermal effects, but proper wavelength selection and parameter adjustment remain crucial for all patients.
Results depend on the treated condition. Tattoo removal and benign pigmented lesion treatments typically provide permanent results, while skin rejuvenation treatments may require maintenance sessions.
Recovery typically involves mild redness and swelling for 24-48 hours, with most patients returning to normal activities immediately. Strict sun protection and gentle skincare are essential during healing.