1. 소개
Acne scarring remains one of the most challenging sequelae of inflammatory acne, affecting an estimated 95% of individuals with a history of moderate to severe acne vulgaris. The psychological and social impact of post-acne scarring often persists long after active breakouts have resolved, creating lasting effects on self-esteem and quality of life. As dermatological science advances, innovative laser technologies continue to revolutionize the landscape of scar management and 피부 재포장 treatments.
1.1 Why Acne Scars Remain a Persistent Skin Concern
Acne scarring develops as a consequence of inflammatory acne lesions that damage dermal collagen and elastic fibers during the healing process. The severity and type of scarring depend on multiple factors including genetic predisposition, inflammatory response intensity, and the depth of tissue involvement. Post-inflammatory hyperpigmentation (PIH) and post-inflammatory erythema (PIE) further compound the aesthetic concerns, creating a complex clinical picture requiring sophisticated treatment approaches. Traditional topical therapies often prove inadequate for established scars, as they cannot address the underlying structural changes in dermal architecture. The persistence of acne scarring creates significant psychological burden, with studies demonstrating correlations between scar severity and depression, anxiety, and social withdrawal among affected individuals.
1.2 The Rise of Advanced Laser Treatments for Skin Resurfacing
The evolution of laser technology has transformed dermatological practice, offering precise, controlled methods for addressing various skin concerns including acne scarring. Modern laser systems provide clinicians with sophisticated tools to target specific tissue layers, stimulate collagen remodeling, and achieve optimal aesthetic outcomes with minimal collateral damage. Fractional laser resurfacing revolutionized scar treatment by creating controlled zones of thermal injury while preserving surrounding healthy tissue, promoting faster healing and reduced downtime. The development of picosecond laser technology represents the latest advancement in this field, offering unprecedented precision and efficacy. These innovations have shifted the paradigm from invasive surgical procedures to minimally invasive laser treatments that deliver superior results with enhanced safety profiles and patient comfort.
1.3 What Makes Pico Laser Different?
Picosecond laser technology distinguishes itself through ultra-short pulse durations measured in trillionths of a second, significantly shorter than traditional nanosecond lasers. This revolutionary timing enables the generation of photoacoustic effects rather than purely photothermal reactions, minimizing heat-related tissue damage while maximizing therapeutic efficacy. The photomechanical disruption created by picosecond pulses effectively shatters pigments and stimulates robust collagen remodeling without the thermal coagulation zones associated with longer pulse durations. Advanced picosecond systems incorporate multiple wavelengths, including 532nm for superficial concerns and 1064nm for deeper tissue penetration, allowing customized treatment protocols for diverse scar types. This technological innovation represents a paradigm shift toward more precise, comfortable, and effective skin resurfacing treatments with superior clinical outcomes.
2. Understanding Acne Scars and Skin Resurfacing
The complexity of acne scarring necessitates a comprehensive understanding of scar classification, pathophysiology, and the limitations of conventional treatments. This knowledge forms the foundation for implementing effective laser-based interventions that address both structural and pigmentary components of post-acne changes.
2.1 Types of Acne Scars
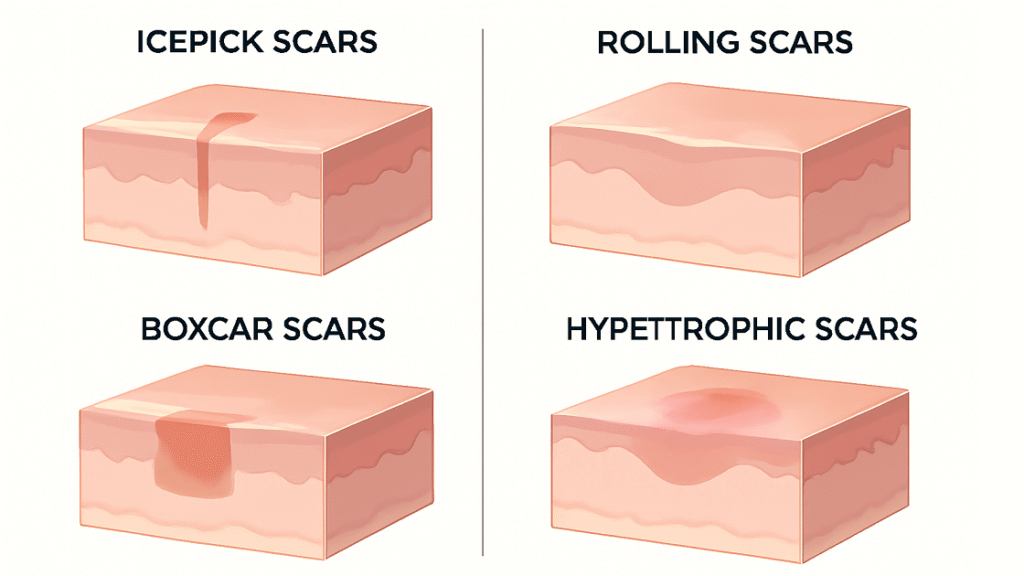
Acne scar classification follows established morphological criteria that guide treatment selection and predict therapeutic outcomes. Atrophic scars, comprising approximately 80-90% of all acne scars, result from collagen destruction during inflammatory healing processes. Ice-pick scars present as narrow, deep depressions extending into the dermis, often measuring less than 2mm in diameter with steep, punched-out appearance. Rolling scars demonstrate wave-like undulations caused by fibrous bands tethering the dermis to underlying structures, creating broader, shallow depressions. Boxcar scars exhibit well-defined edges with flat bases, resembling chickenpox scars and varying in depth from superficial to deep dermal involvement. Hypertrophic scars, less common in facial acne, result from excessive collagen production and appear as raised, firm nodules that remain within the original wound boundaries, contrasting with keloids that extend beyond initial injury sites.
2.2 Why Conventional Treatments May Fall Short
Traditional topical treatments including tretinoids, hydroquinone, and vitamin C serums primarily address superficial pigmentary changes but lack the ability to remodel established collagen architecture in atrophic scars. Chemical peels, while effective for mild textural irregularities and post-inflammatory hyperpigmentation, provide limited penetration depth and cannot adequately address deeper dermal scarring. Microneedling stimulates collagen production through controlled injury mechanisms but requires multiple sessions and may not achieve sufficient remodeling for severe scarring. These conventional approaches often result in modest improvements that fail to meet patient expectations, particularly for moderate to severe scarring. The limitations of traditional therapies stem from their inability to precisely target specific tissue layers while sparing healthy surrounding structures, leading to suboptimal results and potential complications in darker skin types.
2.3 The Science of Skin Resurfacing in Scar Revision
Skin resurfacing operates on fundamental principles of controlled wound healing and collagen remodeling to improve scar appearance and texture. The process involves precise removal or modification of damaged tissue layers, triggering cascades of cellular repair mechanisms including fibroblast proliferation, neocollagenesis, and dermal remodeling. Optimal resurfacing achieves the delicate balance between sufficient tissue injury to stimulate repair while minimizing complications and downtime. The wound healing response following laser resurfacing involves three distinct phases: inflammatory, proliferative, and remodeling, each contributing to the final aesthetic outcome. Cytokine release, growth factor activation, and matrix metalloproteinase regulation orchestrate the complex biological processes that ultimately result in improved skin texture, reduced scar visibility, and enhanced overall appearance.
2.4 Where Pico Laser Fits in Modern Scar Management
Picosecond laser technology occupies a unique position in contemporary scar management by offering precise targeting capabilities with minimal thermal damage. The ultra-short pulse duration enables selective photothermolysis of pigmented lesions while simultaneously stimulating dermal remodeling through photoacoustic mechanisms. This dual action addresses both atrophic scarring and associated pigmentary changes in a single treatment modality, streamlining patient care and optimizing outcomes. Modern scar management protocols increasingly incorporate picosecond lasers as first-line treatments for mixed scar types, particularly in patients with Fitzpatrick skin types III-V who are at higher risk for post-inflammatory pigmentation with traditional resurfacing methods. The technology’s versatility allows for customized treatment protocols that can be adjusted based on scar morphology, skin type, and individual patient factors, positioning it as an essential tool in comprehensive scar revision programs.
3. Pico 레이저란 무엇이며 어떻게 작동하나요?
The scientific foundation of picosecond laser technology represents a significant advancement in dermatological laser physics, offering unprecedented precision and efficacy through innovative pulse delivery mechanisms. Understanding these fundamental principles is crucial for appreciating the clinical advantages and therapeutic potential of this revolutionary technology.
3.1 Picosecond Technology Explained
Picosecond laser technology utilizes ultra-short pulse durations measured in picoseconds (10^-12 seconds), representing a thousand-fold reduction compared to traditional nanosecond systems. This dramatic decrease in pulse duration fundamentally alters the laser-tissue interaction, shifting from predominantly photothermal effects to photomechanical disruption mechanisms. The rapid energy delivery creates intense pressure waves and acoustic phenomena that mechanically disrupt targeted structures while minimizing heat diffusion to surrounding tissues. Advanced picosecond systems incorporate sophisticated beam delivery mechanisms, adjustable spot sizes, and multiple wavelength capabilities to optimize treatment parameters for diverse clinical applications. The technology’s precision allows for selective targeting of specific chromophores while preserving healthy tissue architecture, resulting in superior clinical outcomes with reduced risk of adverse effects and enhanced patient comfort during treatment sessions.
3.2 Mechanism of Action in Skin Resurfacing
The therapeutic mechanisms underlying picosecond laser effectiveness in skin resurfacing involve complex photobiological processes that promote tissue remodeling and regeneration. These mechanisms work synergistically to address multiple aspects of acne scarring simultaneously, providing comprehensive treatment outcomes that surpass traditional approaches.
3.2.1 Collagen Stimulation & Remodeling
Picosecond laser pulses generate photoacoustic waves that mechanically stimulate fibroblasts and activate collagen synthesis pathways without significant thermal coagulation. The mechanical disruption triggers release of growth factors including transforming growth factor-beta (TGF-β), platelet-derived growth factor (PDGF), and vascular endothelial growth factor (VEGF). These signaling molecules initiate cascades leading to increased collagen I and III production, elastin synthesis, and dermal matrix reorganization. The photomechanical effect creates microscopic tissue disruption zones that stimulate wound healing responses while maintaining tissue architecture integrity. This controlled remodeling process continues for several months post-treatment, resulting in gradual improvement in scar texture, depth, and overall skin quality through enhanced dermal thickness and improved collagen organization.
3.2.2 Pigment Shattering for Post-Acne Marks
The ultra-short pulse duration of picosecond lasers enables efficient fragmentation of melanin granules and other pigmented particles through photoacoustic disruption rather than thermal coagulation. This mechanism proves particularly effective for post-inflammatory hyperpigmentation (PIH) associated with acne scarring, where traditional longer-pulse lasers may cause additional inflammation. The mechanical shattering creates smaller pigment fragments that are more readily processed by macrophages and eliminated through lymphatic drainage. Wavelength selection plays a crucial role, with 532nm effectively targeting superficial epidermal melanin while 1064nm addresses deeper dermal pigmentation. The reduced thermal component minimizes risk of paradoxical hyperpigmentation, making picosecond technology safer for darker skin types where pigmentary complications represent significant concerns with conventional laser approaches.
3.2.3 Minimal Thermal Damage & Faster Healing
The abbreviated pulse duration significantly reduces thermal diffusion time, limiting heat spread to targeted structures and minimizing collateral tissue damage. This precision thermal confinement preserves surrounding healthy tissue architecture, resulting in faster healing times and reduced downtime compared to traditional ablative or fractional laser treatments. The minimal thermal damage translates to reduced inflammatory response, decreased post-treatment erythema, and faster epithelialization of treated areas. Patients typically experience mild discomfort during treatment with rapid resolution of acute side effects, allowing earlier return to normal activities. The preserved tissue architecture maintains natural skin barrier function, reducing infection risk and promoting optimal healing conditions that contribute to superior long-term aesthetic outcomes and patient satisfaction.
3.3 Safety Profile of Pico Laser for Acne-Prone and Sensitive Skin
Extensive clinical research demonstrates excellent safety profiles for picosecond laser technology, particularly in patients with acne-prone and sensitive skin conditions. The reduced thermal component minimizes risk of treatment-induced acne flares, a concern with traditional resurfacing methods that can temporarily compromise skin barrier function. Post-treatment inflammatory responses are typically mild and transient, with most patients experiencing only minimal erythema lasting hours rather than days. The technology’s precision allows for safe treatment of active inflammatory lesions while simultaneously addressing scarring, streamlining patient care and reducing treatment timelines. Contraindications remain limited to pregnancy, active infections in treatment areas, and certain photosensitizing medications, making picosecond lasers suitable for most patient populations seeking scar revision treatments with enhanced safety margins.
4. Effectiveness of Pico Laser for Acne Scars
Clinical evidence supporting picosecond laser efficacy for acne scar treatment continues to expand through rigorous research studies and long-term outcome assessments. These investigations provide valuable insights into treatment effectiveness across different scar types and patient populations, establishing evidence-based treatment protocols.
4.1 Evidence from Clinical Studies and Dermatology Trials
Systematic reviews and meta-analyses have evaluated numerous randomized controlled trials demonstrating picosecond laser efficacy for acne scar improvement. A landmark study published in JAMA Dermatology reported significant improvements in acne scar appearance following picosecond laser treatment, with 90% of patients achieving good to excellent results. Prospective studies consistently show superior outcomes compared to traditional fractional lasers, with reduced downtime and enhanced patient satisfaction scores. Clinical trials utilizing standardized assessment tools including the Echelle d’Evaluation Clinique des Cicatrices d’Acne (ECCA) scale demonstrate measurable improvements in scar severity, texture, and overall appearance. Long-term follow-up studies reveal sustained improvements lasting 12-18 months post-treatment, with some patients maintaining benefits beyond two years. These robust clinical data support picosecond laser integration into evidence-based scar treatment protocols.
4.2 Pico Laser Results for Different Acne Scar Types
The versatility of picosecond laser technology enables effective treatment of diverse acne scar morphologies through customized treatment parameters and protocols. Understanding type-specific responses guides treatment planning and patient counseling regarding expected outcomes and treatment requirements.
4.2.1 Atrophic and Ice-Pick Scars
Clinical studies demonstrate excellent results for atrophic acne scars, with average improvements of 50-75% in scar depth and volume following treatment series. Ice-pick scars, traditionally challenging to treat due to their narrow, deep morphology, respond favorably to high-energy picosecond pulses that effectively stimulate collagen production in scar bases. The photoacoustic mechanism creates controlled tissue disruption that promotes fibroblast migration and collagen deposition in previously atrophic areas. Sequential treatments typically show progressive improvement, with optimal results achieved after 3-6 sessions spaced 4-6 weeks apart. Patient selection criteria favor recent scars and younger patients who demonstrate more robust collagen synthesis responses. Combined treatment approaches incorporating picosecond laser with microneedling or radiofrequency enhance outcomes for severe atrophic scarring through complementary mechanisms of action and enhanced tissue remodeling.
4.2.2 Rolling and Boxcar Scars
Rolling scars demonstrate particularly favorable responses to picosecond laser treatment due to the technology’s ability to disrupt fibrous bands and stimulate dermal remodeling. Clinical trials report 60-80% improvement in rolling scar appearance, with patients noting smoother skin texture and reduced shadow effects. Boxcar scars respond variably depending on depth and edge definition, with shallow to moderate scars showing superior outcomes compared to deep, well-demarcated lesions. The treatment protocol typically involves higher fluences and multiple passes to achieve adequate tissue stimulation while maintaining safety margins. Combination approaches incorporating subcision techniques with picosecond laser treatment enhance outcomes for severe rolling scars by addressing both mechanical tethering and dermal volume deficits. Long-term results demonstrate sustained improvement with gradual continued enhancement for 6-12 months post-treatment as collagen remodeling processes mature and optimize skin texture.
4.2.3 Pigmented Post-Inflammatory Marks
Post-inflammatory hyperpigmentation associated with acne scarring responds exceptionally well to picosecond laser treatment, with clinical studies reporting 70-90% improvement in pigment intensity. The technology’s ability to selectively target melanin while minimizing thermal damage makes it ideal for treating PIH in all skin types, including Fitzpatrick IV-VI where traditional lasers carry higher complication risks. Treatment protocols typically utilize lower fluences initially, with gradual increases based on patient response and tolerance. The 532nm wavelength proves most effective for epidermal pigmentation, while 1064nm addresses deeper dermal melanin deposits. Combined treatment of both scarring and pigmentation in single sessions provides comprehensive results, reducing total treatment burden and enhancing patient satisfaction. Maintenance treatments may be required for optimal long-term pigment control, particularly in patients with ongoing inflammatory acne or significant sun exposure.
4.3 Short-Term vs Long-Term Outcomes
Short-term outcomes (4-12 weeks post-treatment) demonstrate rapid improvement in skin texture, pigmentation, and overall appearance, with most patients noting visible changes within 2-4 weeks of initial treatment. Immediate post-treatment responses include mild erythema and subtle skin tightening effects that resolve within hours to days. Progressive improvement continues throughout the treatment series, with cumulative benefits becoming apparent after 2-3 sessions. Long-term outcomes (6-24 months) reveal sustained improvements in scar appearance, skin texture, and pigmentation, with many patients maintaining results beyond initial treatment periods. Collagen remodeling continues for 6-12 months post-treatment, contributing to ongoing improvement even after treatment completion. Long-term satisfaction rates exceed 85% in most studies, with patients reporting enhanced confidence and quality of life measures. Durability of results depends on factors including age, skin type, scar severity, and adherence to post-treatment care protocols.
4.4 Success Rates Compared to Other Treatments
Comparative studies demonstrate superior success rates for picosecond laser treatment versus traditional modalities including chemical peels, microneedling, and fractional CO2 lasers. Head-to-head trials show 20-30% greater improvement in scar severity scores compared to microneedling alone, with significantly reduced treatment discomfort and downtime. When compared to fractional ablative lasers, picosecond technology achieves similar efficacy with markedly improved safety profiles and patient tolerance. Success rates for picosecond laser treatment range from 70-90% depending on scar type and severity, compared to 40-60% for conventional treatments. The technology’s ability to address both atrophic scarring and associated pigmentation simultaneously provides comprehensive results that surpass single-modality approaches. Cost-effectiveness analyses demonstrate favorable outcomes despite higher per-session costs due to reduced treatment requirements and superior patient satisfaction rates.
5. Patient-Centered Benefits of Pico Laser
The patient experience remains paramount in contemporary dermatological practice, with treatment selection increasingly influenced by factors including comfort, convenience, and comprehensive outcome satisfaction. Picosecond laser technology addresses these priorities through multiple patient-focused advantages that enhance treatment acceptability and adherence.
5.1 Non-Invasive and Minimal Downtime
Picosecond laser treatment offers a completely non-invasive approach to acne scar revision, eliminating surgical risks, anesthesia requirements, and extended recovery periods associated with more aggressive interventions. The minimal thermal component significantly reduces post-treatment downtime, with most patients experiencing only mild erythema lasting hours rather than days. Treatment sessions typically require no pre-procedure preparation beyond sun avoidance and appropriate skincare modifications, allowing easy integration into busy lifestyles. Post-treatment activities can usually be resumed immediately, with only basic sun protection and gentle skincare required during the healing phase. This convenience factor proves particularly valuable for working professionals and active individuals who cannot accommodate extended recovery periods. The reduced downtime also enables more frequent treatment sessions if needed, potentially accelerating overall treatment timelines and enhancing patient satisfaction.
5.2 Reduced Risk of Side Effects
The advanced technology and precise targeting capabilities of picosecond lasers significantly reduce the risk of adverse effects compared to traditional resurfacing methods. Clinical studies report side effect rates below 5%, with most complications being mild and self-limiting. The reduced thermal damage minimizes risks of post-inflammatory hyperpigmentation, particularly important for patients with darker skin types who face higher complication rates with conventional laser treatments. Infection risks remain negligible due to the non-ablative nature of most picosecond protocols, eliminating concerns about wound care and bacterial contamination. The precise energy delivery reduces risks of over-treatment and associated complications such as scarring, texture changes, or prolonged healing. This enhanced safety profile makes picosecond laser suitable for a broader range of patients and skin types than traditional resurfacing modalities.
5.3 Faster Recovery and Return to Daily Activities
The minimal tissue disruption associated with picosecond laser treatment enables rapid recovery and immediate return to normal daily activities for most patients. Unlike ablative procedures requiring days to weeks of healing, picosecond treatments typically involve only hours of mild discomfort and temporary redness. Patients can usually apply makeup and resume skincare routines within 24 hours of treatment, facilitating normal social and professional obligations. The absence of open wounds or significant tissue damage eliminates restrictions on exercise, travel, or other activities that might be contraindicated with more aggressive treatments. This rapid recovery translates to reduced indirect costs including lost wages, childcare arrangements, or social limitations that accompany more invasive procedures. The convenience factor significantly enhances treatment compliance and patient satisfaction, contributing to better long-term outcomes through consistent treatment adherence and appropriate follow-up care.
5.4 Improvement in Skin Texture, Tone, and Overall Confidence
Comprehensive improvement in multiple skin parameters contributes to enhanced patient confidence and quality of life measures that extend beyond simple scar reduction. Clinical assessments demonstrate significant improvements in overall skin texture, smoothness, and tactile quality following picosecond laser treatment. Simultaneous addressing of pigmentation concerns creates more uniform skin tone and enhanced radiance that complements scar improvement. Patients consistently report increased confidence in social and professional situations, reduced reliance on concealing makeup, and enhanced comfort with close-up interactions. Quality of life questionnaires reveal improvements in self-esteem, social functioning, and overall psychological wellbeing following successful treatment. The comprehensive aesthetic enhancement addresses the multifaceted nature of acne scarring’s impact, providing holistic improvement that resonates with patients’ treatment goals and expectations. These psychological benefits often prove as valuable as the physical improvements, contributing to overall treatment success and long-term satisfaction.
6. Practical Considerations for Pico Laser Treatment
Successful picosecond laser implementation requires careful attention to patient selection, treatment planning, and comprehensive care protocols that optimize outcomes while maintaining safety standards. Understanding these practical aspects ensures effective treatment delivery and patient satisfaction.
6.1 Who Is a Good Candidate?
Ideal candidates for picosecond laser acne scar treatment include individuals with realistic expectations, stable skin conditions, and commitment to post-treatment care protocols. Patients with Fitzpatrick skin types I-IV typically demonstrate optimal results, though careful parameter adjustment enables safe treatment of darker skin types. Age considerations favor younger patients who maintain robust collagen synthesis capacity, though older individuals can achieve significant improvement with adjusted expectations. Medical history screening excludes patients with active infections, autoimmune conditions affecting wound healing, or current isotretinoin use within six months. Psychological assessment ensures realistic expectations and understanding of treatment requirements, timelines, and potential outcomes. Motivation for treatment compliance, including adherence to sun protection and skincare regimens, significantly influences treatment success and long-term result maintenance.

6.2 Contraindications and Safety Precautions
Absolute contraindications include pregnancy, active skin cancer in treatment areas, and current use of photosensitizing medications that increase adverse reaction risks. Relative contraindications encompass recent isotretinoin use, active inflammatory skin conditions, and history of keloid formation requiring individual risk-benefit assessment. Patients with unrealistic expectations, severe body dysmorphic disorder, or inability to comply with post-treatment care require careful counseling or treatment deferral. Pre-treatment assessment includes comprehensive medical history, medication review, and skin examination to identify potential complications or contraindications. Sun exposure limitations require initiation 4-6 weeks prior to treatment and continuation throughout the treatment period to optimize safety and outcomes. Proper eye protection, patch testing for sensitive individuals, and emergency protocols ensure comprehensive safety measures during treatment delivery.
6.3 Downtime, Aftercare, and Skincare Recommendations
Post-treatment care protocols focus on gentle skincare, sun protection, and monitoring for potential complications while optimizing healing conditions. Immediate post-treatment care involves cold compresses for comfort, gentle cleansing with non-irritating products, and application of bland moisturizers to support barrier function. Sun protection becomes critical for 4-6 weeks post-treatment, requiring broad-spectrum SPF 30+ sunscreen and protective clothing to prevent post-inflammatory hyperpigmentation. Skincare modifications include temporary discontinuation of active ingredients including retinoids, AHA/BHA products, and vitamin C to prevent irritation during healing. Activity restrictions remain minimal, with avoidance of excessive heat, steam, or sweating for 24-48 hours post-treatment. Follow-up appointments monitor healing progress, assess treatment response, and adjust subsequent treatment parameters based on individual response patterns. Patient education regarding expected healing timeline, normal vs. concerning symptoms, and emergency contact procedures ensures appropriate post-treatment management and optimal outcomes.
7. Risks, Side Effects, and Safety Insights
Understanding the potential risks and side effects associated with picosecond laser treatment enables informed consent procedures and appropriate patient counseling while maintaining realistic treatment expectations. The overall safety profile remains excellent with proper patient selection and treatment protocols.
7.1 Common Temporary Side Effects (Redness, Swelling, Mild Irritation)
The most frequently reported side effects following picosecond laser treatment include mild erythema, transient swelling, and temporary skin sensitivity that typically resolve within hours to days. Erythema patterns may follow the treatment grid and generally fade within 2-6 hours post-treatment, occasionally persisting up to 24-48 hours in sensitive individuals. Mild edema may occur, particularly in periorbital areas, and typically resolves spontaneously within 24 hours without specific intervention. Temporary skin sensitivity to temperature changes, skincare products, or environmental factors may persist for 3-7 days post-treatment, requiring gentle care protocols. Some patients experience mild desquamation or fine scaling 3-7 days post-treatment as part of normal cellular turnover acceleration, typically resolving with appropriate moisturization. These predictable responses are generally well-tolerated and rarely interfere with normal activities, contributing to high patient satisfaction and treatment completion rates.
7.2 Rare Complications and How to Avoid Them
Serious complications from picosecond laser treatment are extremely rare but can include post-inflammatory hyperpigmentation, hypopigmentation, and, in very rare cases, scarring. Post-inflammatory hyperpigmentation is more common in darker skin types but can be minimized with proper parameter selection, pre-treatment preparation, and strict sun avoidance afterward. Hypopigmentation is uncommon and usually linked to overly aggressive settings or insufficient cooling, highlighting the importance of conservative treatment approaches. Scarring or textural changes are exceptional events, typically arising from poor candidate selection, excessive energy delivery, or non-compliance with aftercare. Infection risk is minimal due to the non-ablative nature of most picosecond laser protocols, though maintaining good post-treatment hygiene remains essential. Preventive strategies include careful patient screening, gradual treatment escalation, and thorough education on aftercare practices. Finally, having emergency protocols and referral systems in place ensures rapid management of any rare adverse effects, reinforcing the overall safety and reliability of picosecond laser therapy.
8. Key Findings on Pico Laser Effectiveness for Acne Scars
Picosecond laser therapy has emerged as a highly effective, safe, and patient-friendly option for acne scar treatment. Clinical studies show 70–90% success rates, particularly for atrophic scars and post-inflammatory pigmentation, with faster healing and fewer complications compared to traditional methods. The technology’s ultra-short pulse duration produces precise photoacoustic effects, stimulating collagen remodeling and reducing pigmentation while minimizing thermal damage to surrounding tissue. This mechanism enables faster recovery, minimal downtime, and enhanced safety for diverse skin types. Patients benefit from improved skin texture, tone, and confidence, with results often sustained for 12–24 months post-treatment. High satisfaction rates reflect the treatment’s non-invasive nature, reduced side effects, and lifestyle-friendly recovery. As evidence grows, Pico Laser is increasingly positioned as a first-line solution for acne scars, supported by ongoing research refining protocols, combination therapies, and long-term outcomes.